The best thing since sliced bread
This year marks 25 years since the medication imatinib (Glivec) was first used to treat chronic myeloid leukaemia (CML) in New Zealand. Carol Clarke, the first New Zealander to begin taking the game-changing treatment, tells her story.
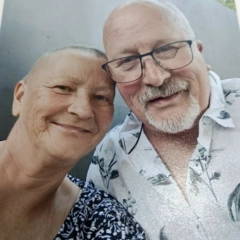
Back in 2000, Carol and her husband Graham were living in Rotorua, where Carol worked as an insurance consultant. Their sons had left home, and the couple had taken up dancing in their free time.
“We were having a lesson one day, and I couldn’t even do one round of the floor,” Carol recalls. “I was just exhausted.”
Carol was 52 at the time. She’d been having night sweats and hot flushes, so she assumed she was probably going through menopause.
Her GP agreed that this was the most likely explanation for her symptoms and suggested hormone replacement therapy. “He said we’d do a blood test now, and another blood test in two months’ time. And then he phoned me at 9 o’clock one Saturday night.”
Concerned with her results, the GP asked Carol if she’d had an infection recently. When she told him she hadn’t, he ordered a repeat blood test for two weeks later. Not long after the second test, Carol was called back into the doctor’s surgery and given the devastating news.
“My GP said he was 99% sure I had CML.”
At the time, CML was treated with interferon and chemotherapy. On average, patients only survived four to five years. Carol was terrified.
“I thought it was a death sentence.”
She was referred to a haematologist, who confirmed her diagnosis, but also offered some promising news. It just so happened that in 2000, a trial for imatinib, a new drug to treat CML, was starting in New Zealand. Carol was diagnosed in April, and the trial was due to start in October.
To be eligible for the trial, Carol must not have tried any previous treatments. As she waited for the trial to start, her blood test results continued to worsen. “My doctor said to me, ‘Carol, your blood counts are going up. I don’t think you should wait for the trial.’ And I told him, ‘I’m going to wait.’”
On 22 October, 2000, Carol took her first dose of imatinib, making her the first Kiwi patient to trial the drug.
Within just six months, she was in remission.
“It was splashed all over the paper, and I thought, ‘What’s all this fuss about?’ But it had been the biggest breakthrough in about 25 years, apparently. The best thing since sliced bread.”
That’s not to say it was all plain sailing.
“The side effects were pretty harsh – I had puffy eyes and my hair went very thin – but it saved my life.”
Carol continued taking imatinib for 17 years. Life continued as normal – her energy returned and she kept working, only taking the odd day off for doctors’ appointments.
Then one day in 2017, Carol collapsed. After being rushed to the hospital, it was discovered she was bleeding internally and needed urgent surgery. “The doctor who did the operation said to me, ‘You had absolutely nothing left.’ My haemoglobin was in the 60s or 70s.”
Once she was stable, it was suggested to Carol that her medication might have been the cause of the bleeding. “They said to me they were going to take me off it, and I got very nervous then, thinking, ‘Gosh, I’ve been on it for so long. Is the leukaemia just going to come back rampant again?’”
She sought a second opinion from another haematologist, who agreed that stopping treatment was the right decision.
“So I came off it, and here I am – still here!”
Carol still gets blood tests every three months to keep an eye on things, but so far, her CML has stayed under control.
Devastatingly, Carol recently lost Graham after 58 years of marriage. Adjusting to life without him has been tough, but she’s got great family and friends who have rallied around her.
After living in Rotorua for 40 years, she now lives in Cambridge and enjoys going along to her local LBC support group. “Everybody else has had the same thing or is going through some sort of treatment,” she says. “They’re nice ladies.”
25 years on from when she was first diagnosed, Carol is aware that things could have taken a very different path if she’d been diagnosed even just a year earlier.
“If I had to get CML, I got it at the right time.”
She doesn’t take the time she’s been given for granted. “I really didn’t think I would last 25 years, to be quite honest. Somebody’s looking after me!”